General Toxicology
Written by Dr. D. Rao
General Toxicology
TOXICOLOGY-GENERAL
A poison is a substance (solid, liquid or gaseous), which introduced into the living body or brought into contact with any part there of, will produce ill-health or death, by its constitutional or local effects or both.
The intent with which any act is committed is an important element in law, Administration of any substance with the intention of causing injury of death and which causes injury or death as a result, is legally sufficient for awarding punishment, whether the substance is one which can be called poison or not. Administering poison to a person with criminal intent is by itself a criminal offence, whether actual hurt is caused or not.
Criminal Offences: The administration of poison is a criminal offence whenever:
- It is with intent to kill.
- With intent to cause serious injury.
- Used recklessly even though there is no intent to kill.
- For stupefying to facilitate a crime, e.g., robbery or rape.
- To procure an abortion.
- To annoy the victim.
- To throw poison at another person with intention to injure him.
Causes of Poisoning:
- The administration of poison for criminal purposes.
- The swallowing of poison in mistake for innocuous substance.
- The inhalation through ignorance or accident, of the vapours of a poison.
- The incorrect compounding of medicines containing a poison.
- The accidental taking of a large dose of medicine containing a poison.
- Excessive self-medication.
- Addiction to drugs.
- Bite by a poisonous animal.
- Food infected with bacteria or their toxins.
Poisoning and the Pathologist
The pathologist is concerned with evaluating poisons as a cause or contribution to death.His main task is to confirm or exclude other nontoxic factors in the death.He has to collect suitable samples for analysis and, when the laboratory results are available to interpret them in the light of his knowledge of the history,clinincal features and autopsy appearances.
Signs and symptoms of poisoning:
- The symptoms appear suddenly in a healthy person.
- The symptoms appear immediately or within a short period after food or drink.
- The symptoms are uniform in character and rapidly increase in severity.
- When several persons partake at the same time in the same source of poison, all suffer from similar symptoms at or about the same time.
- The discovery of poison in food taken, in the vomit or in the excreta is strong proof of poisoning.
Collect (1) Stomach wash. (2) 10 ml. of blood. (3) Urine. (4) Faeces.
10 mg. of Sodium fluoride for 10 ml. of blood acts both as a preservative and as an anticoagulant.
DIAGNOSIS IN THE DEAD: Investigation of drug deaths involves team work.
- Investigator should observe for (a) drugs available, (b) circumstances, (c) appearance and position of body.
- Pathologist must do a complete autopsy to: (a) recognize drug cases, (b) collect proper specimens, (c) lend direction to toxicologist.
- Toxicologist should (a) review case with Pathologist, (b) analyse in orderly manner, (c) discuss interpretation of findings with Pathologist.
- PRELIMINARY STEPS: Scene of death:
- History of suicidal tendencies or previous attempts at suicide.
- Check for glasses, bottles, tablets, capsules, etc.
- Look for suicide notes.
- Note the appearance and position of the body.
-
Ascertain when deceased was last seen alive.
- Deaths occurring after hospitalization:
- Check clinical course for compatibility with drug overdose.
- Find out if stomach wash was done.
- Find out if any blood sample has been taken.
-
Check the record for reports of drug levels.
- Suspected death from Drugs:
- In cases where the history suggests involvement of drugs.
- Deaths in teenagers and young adults without a history of pre-existing serious disease.
In most poisonings the major function of the autopsy is to evaluate any other conditions present, both from trauma and natural disease-but also to collect suitable material for laboratory analyis.The proper retention of optimal samples, their correct preservation and dispatch to the Toxicologist is of fundamental importance.
II. AUTOPSY: (A) EXTERNAL:
- The surface of the body and clothes may show stains or marks of vomit, faeces or the poison itself. Dark brown stains about the lips, chin, cheeks etc. are suggestive of burning by corrosives.
- Color of post-mortem staining: The skin may be yellow in phosphorus and acute copper poisoning. Cherry red staining suggests poisoning by carbon monoxide. Bright red staining is seen in hydro cyanic acid poisoning. In poisoning by nitrates, potassium chlorate and aniline the color is brown or deep blue.
- Smell about the mouth and nose. Compress chest and inhale near nose. Substances which may be recognized by their odor are alcohol, ether, chloroform, cyanides, phenol, opium, organ phosphorus compounds, endrin, camphor, paraldehyde, etc.
- The natural orifices may show the presence of poisonous material or the signs of its having been used.
- Injection marks should be looked for with care.
- Look for old scars from previous suicide attempts.
- Look for blisters on extremities from barbiturates, sedatives, carbon monoxide, etc.
(B). INTERNAL:
- Smell: On opening the body notes any peculiar smell. It will be strongest in the stomach.
- Mouth and throat: Examine for any evidence of inflammation, erosion or staining.
- Oesophagus: Corrosives produce marked softening and desquamation of the mucous membrane.
- Upper respiratory tract: Examine for evidence of volatile irritants or inhaled poisonous matter. Laryngeal oedema is usually found in alcohol and barbiturate poisoning.
- Lungs: Congested and oedematous in most cases. Laryngeal oedema is usually seen in deaths from alcohol and barbiturates.
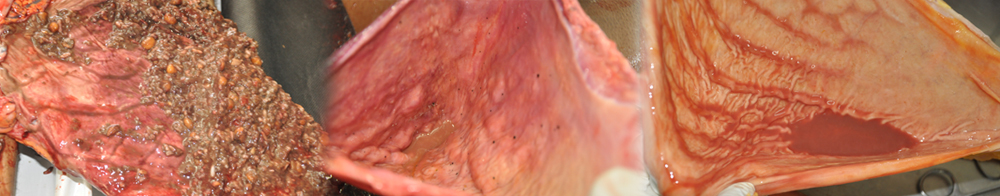
- STOMACH: (a) Hyperaemia is caused by an irritant poison, is usually marked at the cardiac end and greater curvature of stomach. It is usually patchy and of a deep crimson colour. The ridges are more involved. The ridges are more involved. The mucous membrane is often covered with a viscid secretion and shows small haemorrhagic foci. (b) Softening: Corrosives and irritants damage the epithelium. Excess of mucus is secreted. Softening of mucous membrane especially at its cardiac end and greater curvature of the stomach. It appears as an erosion with thin friable margins. The surrounding mucosa is softened due to inflammation and there is diffuse hyperaemia. (d) Perforation: It may occur in sulphuric acid poisoning. The stomach is blackened and extensively destroyed. The aperture is irregular, the edges sloughing and the adjacent tissues easily torn.
- Liver: Arsenic, phosphorus and rarely ferrous sulphate produce a fatty yellow liver. Arsephenamine, chloroform, carbonate-tetrachloride, etc., may produce liver necrosis.
- Kidneys: Degenerative changes are usually found in irritant metal poisoning and in cantharidine poisoning. Extensive necrosis of proximal convoluted tubules may be found in poisoning by mercury, phenol and carbontetrachloride.
- Heart: Sub-endocardial haemorrhages in the left ventricle occur in most cases of acute arsenic poisoning.
- Brain: May show swelling or pressure cone. There may be symmetrical necrosis of basal ganglia.
- Bladder: It is usually distended, and often the only clue to death from drugs.
- Vagina and Uterus: Should be examined for the effect of poison in criminal abortion.
- Intravascular: Sickling may be triggered by drug ingestion.
Collection of Autopsy samples for Toxicological analysis.
The investigation of a death from suspected poisoning may stand or fall upon the correctness or otherwise of the sampling of fluids and tissues from the body.Unsuitable samples,inadequate amounts,incorrect sampling sites,and delayed or unsatisfactory storage and transport to the Laboratory may frustrate or distort proper analysis.the final outsome may be wrong,either failing to detect poison actually present,in measuring only part of that originally present or in some cases-even producing falsely high results that then lead to an incorrect cause of death.Not only most samples be in the optimal condition,but the accompanying information from the pathologist in analyst needs to be as accurate and comprehensive as possible,so that the most appropriate techniques are used,and allowance made for any interfering substances which may be present.
Time of sampling
When an autopsy cannot be performed quickly after death,interms of few hours,then mortuary refregiration is the first line of defence to slow up putrefactive and autolytic processes.If delay is forseen,usually because of administrative problems in obtaining consent or authority for autopsy,it may be possible to obtain a sample of blood through the body surface,such as puncturing the femoral vein by needle and syringe.The blood can be kept in optimal condition,with preservatives where needed,and perhaps with the serum or plasma separated from the cells to avoid hemolysis.Similarly,urine could be drawn off by catheter or even suprapubic puncture,unless strict regulations,forbid this as anticipating autopsy permission.
Collection of Specimens:
- Stomach and its contents. Open along lesser curvature. Examine wall for fragments of adherent poison. (a) Measure contents. (b) Look for tablets or capsules. (c) Preserve whole contents if small amount is present; if there is a large amount, take an aliquot.
- Upper part of small intestine and its contents.
- Liver 100-200gm,.
- Kidney: 50gm from each Kidney.
- Blood: 30 ml. from the heart. Do not mix with pericardial fluid and do not collect from the chest cavity.
- Urine 30 ml.
Special Procedures:
- Narcotic poisoning: Collect bile and one-half of one lung
- Inhalation poisons: (a) Tie trachea, (b) collect bronchial air. (c) Collect entire lung and keep in airtight container.e.g.Nylon with out preservatives.
- Pesticides: Fatty tissue from abdominal wall or perinephric region and brain.
- Heavy metals: Hair, nails and bone.
- Pneumoconioses: lung.
- In deaths from extensive trauma: Vitreous fluid for alcohol.
Containers
- Clean containers void of any ingrediadents.
- Blood -30ml Screwcapped containers or 5ml plastic-capped containers.
- Bile/Urine-Universal Containers
- Stomach(wall and contents)-250ml plastic or glass jars lid tight screw thread.
- Intestine(contents)/Liver-Few hundred grams-Larger plastic or glass container.
- Vitreous Humour/CSF small bijou bottles-5ml capacity used.
- Lungs-nylon bag used (solvent abuse or volatile poison).
Suitable Preservatives added with samples and anticoagulants added
Homicidal Poisoning:
- Take extra care to avoid cross-contamination during collection of specimens.
- Prove route of administration. (a) Collect sample of air and lungs. (b) Excise injection site including skin, fat, muscle (take control from the opposite side).
- Verify the drug by as many analytical methods as possible.
- Rule out all possible unrelated causes of death.
- Take sample of hair, nails, bone, etc.
- Maintain chain of possession.
III. Chemical Analysis: Prevent contamination of the solid viscera with the contents of the gastro-intestinal tract, because an idea of the length of time since ingestion may be had from the relative amounts of poison in the stomach, intestines and the solid organs. If the poison is only found in the contents of stomach and none in the solid organs and is not an irritant, doubts may be thrown on the actual cause of death. Poison found in a viscus (other than stomach or intestine) is proof of absorption.
(IV) Animal Experiments.
(V) Circumstantial Evidence: Consists of motive, the evidence of witnesses about the recent purchase of the poison, his behavior before and after the commission of the offence, and the recovery from the possession of the accused or the premises of a poison.
Cause of Death: The blood level of the drug or chemical is useful to determine the cause of death, in correlation with other findings. The blood level of a drug need not always be in the lethal range for it to reflect the cause of death, especially in a treated case. Low levels may be due to passage of time after ingestion with resulting metabolism of drug. Less than lethal levels of drug may trigger other mechanisms of death, e.g., (a) Positional asphyxia, (b) intravascular sickling in certain haemoglobinopathies, (c) post-ictal respiratory failure. When the presence of a highly toxic material is established, even in trace amounts, the inference that the poisoning is the cause of death is justified.
Death may occur 1 to 2 weeks after ingestion of drugs from apparent unrelated causes, e.g., (a) Bronchopneumonia. (b) The rapeutic from tracheostomy. (c) Hepatitis. (d) Fungal or bacterial endocarditis. (e) Encephalomalacia. (f) Haemotologica problems.
No Poison Found: Cases are observed in which no trace of poison is found on analysis, although from other circumstances it is almost or quite certain that the poison was the cause of illness or death. The possible explanations of negative findings are (1) The poison may have been eliminated by vomiting and diarrhoea, e.g., in irritant poisons. (2) The whole of the poison has disappeared from the lungs by evaporation or oxidation, (3) The poison after absorption may be detoxified, conjugated and eliminated from the system. (4) Some vegetable alkaloidal poisons cannot be definitely recognized by analytical methods. (5) Some substances, e.g., toxins of tetanus or salmonella cannot be detected chemically. (6) Some organic poisons especially alkaloids and glucosides may be oxidation during life or due to faulty preservation, or a long lapse of time, or from decomposition of the body may deteriorate and cannot be detected chemically. (7) Many drugs present in very small amounts may require considerable amounts of viscera for identification. (8) The wrong or insufficient material may have been sent for analysis.
Precautions:
- Do a complete autopsy in every case, including microscopic examination.
- If viscera are sent for chemical examination, keep the cause of death pending till the report is received.
- Give the cause of death as due to drugs, after considering investigator’s report, autopsy protocol, laboratory and microscopic reports.
- If low levels are found in viscera, consider: (a) Poly-pharmacy. (b) Time lapse after ingestion with resulting metabolism of drug. (c) Positional asphyxia. (d) Intravascular sickling in certain haemoglobinopathies. (e) Postictal respiratory failure.
- If the victim survives for a week or two, do not give cause of death as bronchopneumonia, but give as bronchopneumonia following drug ingestion.
- Consider all factors, to determine manner of death.
- Maintain chain of custody.
HOUSEHOLD POISONS
DOMESTIC POISONS:
|
Preparation |
Toxic substance |
|
Cosmetics |
|
|
Cuticle remover: |
Potassium hydroxide, trisodium phosphate |
|
Depilatories |
Barium sulphide; thallium |
|
Hair wave lotion |
Thioglycollate salts; perborates; bromates |
|
Nail polish removers |
Acetone |
|
Sun-tan lotions |
Denatured alcohol; methyl Salysilate.
|
|
Baby powder: |
Boric acid. |
|
|
|
|
Kitchen |
|
|
Baking powder |
Tartaric acid 50% |
|
Baking soda |
Sodium bicarbonate |
|
Dish washing compounds |
Sodium polyphosphates; sodium carbonate, sodium silicates.
|
|
Fire extinguishing fluids |
Carbon tetrachloride; sodium carbonate; methyl bromide.
|
|
Matches |
Antimony; Phosphorus; sesqui- sulphide, potassium chlorate |
|
Rat Poisons |
|
|
Rat paste |
Aluminum phosphide; zinc phosphide; Arsenious oxide; red squill; thallium sulphate |
|
Rodine |
Yellow phosphorus |
|
Cockroach Powder |
Yellow phosphorus |
|
Sanitary |
|
|
Deodorant tablets |
Formaldehyde; naphthalene |
|
Drain cleaners |
Sodium hydroxide |
|
Disinfectants: |
Phenol; bleaching powder. |
|
|
|
|
Miscellaneous |
|
|
Insecticide spray |
D.D.T., Gammexane, etc |
|
Moth Balls: |
Naphthalene |
|
Marking ink: |
Aniline |
|
Ink remover |
Sodium hyphochlorite 5% |
|
Anti-rust products: |
Ammonium sulphide, hydrofluoric acid,naphtha, oxalic acid |
|
|
|
|
Cleaning solvents |
Petroleum hydrocarbons; carbon tetrachloride; trichloroethylene |
|
Flourescent lamps |
Beryllium |
|
Furniture Polish |
Turpentine; petroleum hydrocarbons |
|
Paint remover |
Sodium hydroxide; lead acetate |
|
Shoe polish |
Aniline; nitrobenzene |
|
Hair bleach |
Potassium permanganate; hydrogen- Peroxide. |
|
Toys (paints): |
Lead |
|
Fire works |
Arsenic; mercury; antimony; lead, phosphorus; thiocyanate |
|
Crayons (chalk): |
Salts of arsenic, copper, lead |
|
Crayons (wax): |
Para-nitro-aniline |
|
GARDEN POISONS |
|
|
Insecticides |
Organophophorus compounds; chlorinated hydrocarbons; nicotine; Tar oils. |
|
Fungicides |
Lead arsenate; copper Compounds; organic mercurial; Lime sulphur |
|
Weed killers: |
Sodium chlorate; arsenious oxide, and arsenites; dinitrocresol; paraquat |
A.THERAPEUTIC POISONS:
| 1) Antiseptics: | Iodine, benzoin. |
| (2) Tonic tablets: | Iron. |
| (3) Tonic syrup: | Strychnine |
| (4)Sleeping tablets: | Barbiturates |
| (5)Head ache tablets: | Aspirin. |
| (6)Cough remedies: | Codeine |
| (7) Throat tablets: | Potassium chl |
| (8) Pep tablets: | Benzedrine. |
| (9) Others: | Antidepressants; tranquillizers. |
Systemic Toxicology
Written by Dr. D. Rao
SULPHURIC ACID:
Fatal Dose: 10 to 15 cc; Fatal period: 18 to 24 hours.
Autopsy:
- The clothes may show burns and stains.
- Corrosion of mucous membranes of lips, mouth, throat and of the skin over the chin, angles of the mouth and hands is seen.
- The necrotic areas are at first grayish white but soon become brown or black and leathery.
- Internal changes are limited to the upper digestive tract and the respiratory system.
- The upper digestive tract is inflamed and swollen by oedema and severe interstitial haemorrhage. The greater part of stomach may be converted into a soft boggy, black mass which readily disintegrates when touched. The mucosal ridges are more damaged than the furrows. In the damaged areas the mucosa is brown or black. Perforation may occur with escape of stomach contents into the peritoneal cavity. The small intestine may show signs of irritation.
- Corrosion or severe inflammation of the larynx and the trachea may be present.
M L Aspects: (1) Most cases are suicidal. (2) It is not used for homicide. (3) Accidental cases are rare.
NITRIC ACID: Autopsy: (1) Findings are similar to those of Sulphuric acid but, the tissues are stained yellow. (2) Perforation of the stomach is not common. In death from inhalation of fumes, the larynx, trachea and bronchi are congested and lungs are oedematous.
HYDROCHLORIC ACID: Autopsy: (1) Findings are similar to Sulpuric acid, but, corrosion is less severe. (2) Perforation of stomach is rare. (3) Acute inflammation and oedema of respiration tract and lungs are common.
VITRIOLAGE: Throwing of strong corrosive on another person is known as vitriolage. It causes penetrating burns. Repair is slow and scar tissue causes contracture.
CARBOLIC ACID: Fatal dose: 10 to 15g. Fatal period: 3 to 4 hours.
- Corrosion of the skin has a grayish or brown colour.
- The tongue is white and swollen, and there is smell of phenol about the mouth.
- The mucous membrane of the lips, mouth and throat is corrugated, sodden, whitened or ash-grey and partially detached with numerous small submucous haemorrhages.
- The mucosa of the oesophagus is tough, white or grey, corrugated and arranged in longitudinal folds. The stomach is hardened and has a leathery feel. The mucosal folds are swollen and covered by opaque-grey or brown mucous membrane. There may be partial separation of necrotic mucosa.
- The upper part of small intestine may show similar but mild changes.
- The liver and spleen usually show a whitish m hardened patch where the stomach has been in contact with them.
- The brain is congested and may be oedematous.
M. L. aspects: (1) It is used for suicide. (2) Homicide and accident are rare.
CAUSTIC ALKALES
Fatal Dose: 5 to 30g. Fatal period: About 1 day.
Autopsy:
- Alkalies produce soft, oedematous, translucent, soap-like, swollen eschar, red brown in colour.
- The sloughs are mucilaginous.
- Charring is not seen.
- Lips, mouth and throat show corrosion.
- Oesophagus and stomach show inflammatory oedema with corrosion and sliminess of the tissues. Mucosa may be brownish. Perforation of the stomach is rare.
ORGANOPHOSPHORUS POISONS
They are absorbed by inhalation, intact skin, mucous membrane, and the gastrointestinal tract.
Fatal dose: Parathion 80 to 175 mg; malathion and diazinon 1g. orally.
Fatal period: 3 to 6 hours.
Autopsy:
- Signs of asphyxia are found.
- Blood stained froth is seen at the mouth and nose.
- The mucosa of the stomach is congested with sub-mucous petechiael haemorrhages. The stomach contents may smell of kerosene.
- The lungs are congested, oedematous and show sub pleural petechiae.
- The internal organs are congested and brain oedematous.
M. L. Aspects: (1) Suicide: Common. (2) Homicide. And Accidental deaths may occur.
ENDRIN
Fatal dose: 5 to 6 G. Fatal period: 1 to 2 hours.
Autopsy:
- Signs of asphyxia are found.
- Blood stained froth may be seen at the mouth and nose.
- The mucosa of respiratory passages is congested and is covered with a blood stained frothy mucus.
- The stomach contents may smell of kerosene.
- The lungs are voluminous, congested and oedematous.
- The internal organs are congested.
M. L. Aspects: (1) Suicide is very common. (2) Homicide is rare, but it is sometimes given mixed with food, sweets or alcohol.
OPIUM
Fatal dose: Opium 2 G.; morphine 0.2G.
Fatal period: 6 to 12 hours.
Autopsy:
- Signs of asphyxia are prominent.
- Froth is seen at the mouth and nose.
- Smell of opium is noted on opening the chest.
- Stomach may contain small lumps of opium.
- Lungs are congested and oedematous.
- Internal organs are congested.
M. L. Aspects: It is an ideal suicidal poison. Homicide is rare.
BARBITURATES
Fatal dose: Short acting 1 to 2 G; medium acting 2 to 3G; long acting 3 to 4G.
Fatal period: One to several days.
Autopsy:
- Signs of asphyxia are seen.
- White particles of barbiturates may be seen in the stomach with mucosal congestion.
- Lungs are congested and oedeematous.
- The brain is oedematous with softening of globus pallidus and multiple punctate haemorrhages into the white matter.
- Internal organs are congested.
M. L. Aspects: (1) It is ideal suicidal poison. (2) Homicide is rare.
CHLORAL HYDRATE
Fatal dose:3 to 5g.
Fatal period: 8 to 12 days.
Autopsy: (1) Gastric mucosa is softened, reddened and eroded and smells of chloral hydras. (2) Brain and lungs are congested.
FOOD POISONING
- In the infectious type the organisms belong mainly to the Salmonella group. Other organisms like Streptococci, Proteus, Coli group and Shigella are also involved.
- The toxic type is due to the ingestion of preformed toxins in prepared food, such as, canned or preserved food. Exotoxins e.g. enterotoxins of staphylococci and Botulinum toxin, produce intoxication.
It may occur as isolated cases or small outbreaks.
Autopsy: (1) The mucosa of the stomach and intestines is swollen and is often intensely congested, and there may be minute ulcers. (2) Liver shows fatty change.
Diagnosis: (1) History. (2) Clinical features. (3) Isolation of the organism from the suspected food and from vomit, faeces, blood, etc., from sick persons. (4) Animal experiment.
BOTULISM
Autopsy: (1) Kidneys, liver and meninges are congested. (2) Histological examination of the organs may show thrombosis.
Diagnosis: History. (2) Clinical features. (3) Demonstration of the toxin in the suspected food. (4) Isolation of the bacillus from the food. (5) Isolation of the toxin in the blood and tissues. (6) Isolation of the bacillus from the patient’s faeces or vomit.
CYANIDES
Fatal dose: Pure acid 50 to 60mg; Sodium or Potassium cyanide 200 to 300mg.
Fatal period: Pure acid, 2 to 10 minutes. Potassium or sodium cyanide ½ an hour.
Autopsy:
- The eyes may be bright, glistening and prominent with dilated pupils.
- The jaws are firmly closed and there is froth at the mouth.
- The colour of the post-mortem staining is bright red.
- Blood stained froth may be found in the trachea and bronchi.
- There is congestion of viscera and oedma of the lungs.
- All the vessels of the body including the veins contain arterial blood.
- The mucosa of the stomach and intestines is often red and congested.
- Cyanide salts produce slight corrosion of mouth.
M. L. Aspects: (1) They are used for suicide, (2) Homicide is rare.
CARBONMONOXIDE
- A cherry red colour of skin, mucous membranes, areas of post-mortem staining, blood, tissues and internal organs is the prominent feature.
- The blood is fluid. Hyperaemia is general and serous effusions are common.
- Fine froth may be seen at the mouth and nose.
- Anoxic skin blebbing are common.
- Lungs are congested and edematous.
- Necrobiosis of the heart muscle and pleural and pericardial haemorrhages are common.
- Bilateral symmetrical necrosis of the Globus pallidius and punctate haemorrhages in the white matter of brain with widespread oedema are common.
M. L. Aspects: (1) Deaths are usually accidental.
(2) Suicide and homicide is rare.
ALCOHOL
Alcohol is a stimulant, but is a selective depressant especially, of the higher nervous centres which it inhibits. It is a hypnotic and diaphoretic.
Fatal dose: 200 to 300 ml. of absolute alcohol consumed in one hour.
Fatal period: 12 to 24 hours.
Alcohol Concentration and Clinical Effects
|
Blood Alcohol
Mg.% |
Effects on Drinkers |
|
|
Inexperienced |
Experienced |
|
|
0-50 |
Not noticeable |
Not noticeable |
|
50-100 |
Slight |
None to slight |
|
100-150 |
Under the influence |
Slight |
|
150-200 |
Drunk |
Under the influence |
|
200-250 |
Drunk to very drunk |
Influenced to drunk |
|
250-300 |
Very drunk |
Drunk to very drunk |
|
300-400 |
Stupor to coma |
Very drunk to stupor |
|
400-500 |
Comatose to death |
Comatose to death |
- Slight effects: Flushed face; dilated pupils; euphoria; loss of restraint.
- Under the influence: “Under the influence” means that due to drinking alcohol a person has lost (to any degree), some of the clearness of the mind and selfcontrol that he would otherwise possess. The symptoms are; Flushed face, dilated and sluggish pupils; euphoria; loss of restraint; thickness of speech; carelessness and recklessness; incoordination; stagger on sudden turning.
- Drunk: The word “Drunk” means that the person concerned was so much under the influence of alcohol as to have lost control of his faculties to such an extent as to render him unable to execute safely the occupation in which he was engaged at the material time. The symptoms are : Flushed face dilated and inactive pupils; rapid movement of eye balls; unstable mood; loss of restratint; clouding of intellect; thickness of speech; incoordination; staggering gait with reeling and lurching when called upon to make sudden turns.
- Very Drunk: Flused or pale face; pupils inactive; contracted or dilated; mental confusion; gross incoordination; slurred speech; staggering; reeling gait; tendency to lurch and fall, vomiting.
- Coma: Rapid pulse, subnormal temperature; stertorous breathing; deep unconsciousness; contracted pupils; but stimulation of the subject, e.g. by pinching or slapping cause them to dilate with slow return.
Medical Examination:
- Consent: It is necessary, preferably written. If the person is unconscious or unfit to give consent the doctor should examine the patient to decide whether immediate medical treatment is necessary and, if so, to make the necessary arrangements. He should not disclose to the police information he obtained during his examination, but should wait to seek the consent of the patient when he regains consciousness or is in a fit condition to be asked. When a person is arrested by the police, the doctor can examine such person without consent, even by using reasonable force if the examination is requested by a police officer not below the rank of Sub inspector (Sec. 53, Cr. P.C.).
- Note preliminaries, e.g., age, sex, address etc., identification marks, etc.
- Note date and time of examination at the beginning and at the end of the examination.
Scheme of Examination:
- Exclusion of injuries and pathological states: (a) Severe head injuries. (b) metabolic disorders, e.g., hypoglycaemia, uraemia. (c) Neurological conditions, e.g., intracranial tumours, epilepsy, acute aural vertigo. (d) Drugs: insulin, morphine, barbiturates, antihistamines, atropine. (e) High fever. (f) Exposure to carbon monoxide.
- History: The history of the relevant events should be obtained from the accused person while observing him. Enquire whether he suffers from any disease or disability or he is under medical treatment.
- General behaviour: (a) State of dress for presence of slobber on mouth or clothing, soiling of clothes by vomit or incontinence. (b) Speech: Note the type, e.g., is it thick, slurred or over precise. Slight blurring of certain consonants is one of the earliest signs of in-co-ordination of the muscles of the tongue and lips. (c) Self Control.
- Memory and mental alertness: (a) The memory of the person for recent events and his appreciation of time can be judged by asking suitable questions about movements during the preceding few hours. A few very simple sums of addition or subtraction may be asked.
- Writing: Ask him to copy a few lines from a newspaper or book and note: (a) the time taken, (b) repetition or omission of words, letters or lines, (c) ability to keep letters in a line, (d) ability to read his own writing.
- Pulse: It is rapid and is usually full and bounding.
- Temperature: The surface temperature is usually raised.
- Skin: It is flushed.
- Mouth: Note the smell of breath.
- Eyes: (a) General appearance: Whether the lids are swollen or red and conjunctivae are congested. (b) Visual acuity: note any gross defect. (c) Intrinsic muscles: (i) Pupils: note whether dilated or contracted. (ii) Reaction to light: Note whether the action is brisk, slow or absent. (d) Extrinsic Muscles: (i) Convergence. (ii) Strabismus. (iii) Nystagmus. The presence of fine lateral nystagmus indicates intoxication.
- Gait: Ask the person to walk across the room and note: (a) Manner of walking: is it straight, irregular, overprecise, staggering or reeling. (b) Reaction time to a direction to turn: Does he turn at once or continues for one or two steps before turning. (c) Manner of turning: Does he keep his balance, lurch forward, or reel to one side.
- Stance: Note whether the person can stand with his eyes shut and heels together without swaying.
- Muscular coordination: Ask to perform: (a) placing finger to nose. (b) Placing finger to finger, (c) picking up medium sized objects from the floor, (d) unbuttoning and rebuttoning shirt.
- Reflexes: Test knee and ankle reflexes which are delayed or sluggish.
- Pulmonary, cardiovascular and alimentary systems: They should be tested and blood pressure taken for the presence or absence of diseases.
Laboratory Investigation: The degree of intoxication can be estimated by the concentration of alcohol in the breath, saliva, blood or urine. Blood is the most suitable and the most direct evidence of the concentration of alcohol in the brain.
Collection of blood: Do not use spirit for cleaning the skin. The skin can be cleaned with 1:1000 mercuric chloride or by washing with soap and water. Draw 5cc. Blood and place in a small bottle which should be tightly closed. 5 mg. of sodium fluoride acts as preservative and anticoagulant. The sample should be refrigerated if not sent immediately for examination.
Precautions:
- Use clean containers with adequate preservative.
- Refrigerate samples while storing.
- Obtain samples with a clean needle and syringe from the femoral or subclavian vessels or heart. Take samples from more than one area if postmortem diffusion is a possibility.
- Spinal fluid and vitreous humor are very good samples.
- Do not take samples from pericardial sac or from the chest cavity.
- Do not use contaminated needles, syringes or containers.
- Do not use spirit for cleaning the skin, before obtaining blood sample.
Alcohol after death: Alcohol diffuses through the intact stomach wall after death into surrounding blood tissues. The concentration of alcohol in the blood after death does not change until alcohol is produced as decomposition begins. If alcohol is found in urine at autopsy, the ingestion of alcohol prior to death is indicated.
Feature of Chronic alcoholism
- Acute fatty liver
- Cirrhosis of the liver with ascites
- GI hemorrhage from bleeding esophageal varices
- Bleeding peptic ulcers
- Pulmonary TB
- RT infection-bronchitis, bronchopneumonia
- Acute pancreatic
- Aspiration of gastric contents with aspiration pneumonia
- Malnutrition
- Alcoholic Cardio Myopathy
- Hypothermia
Morphine (Heroin)
Scene Investigation
- Decedent – Usually a young adult (<30) male, laborer or unsociable workers
- Site of death: Usually a concealed spot with maximum privacy a closed room, location or bathroom, hallway; The decedent is usually on a bed, floot, sofa or chair.
- Addicts paraphernalia: commonly turned at the scene of death are disposable plastic syringe previously used disposed of medicine dropper with tip titled to hypodermic needle, towniguest, matches, spoon, bottle cap, cotton, water.
- Drug: The powdered drug is frequently mixted with lactose mannitol of quinine before use,
External Examination
- Fresh needle punctures on antecubital force on arm, forearm, hands, femoral area, buttom, fugulas area on feat.
- Contusion asnud recent needle punctures.
- Dark brown pigment scary of kolnds due to needle punctures in the part (sometimes in a row) on antecubital fona, arm, forearm, hand. Temoral vein area, buttoc of on jugules are
- Tattoos at the sites of needle puncture of scari ( Imprinted to conceal sites)
- Ropelike thickened virus with or without knots caused by thrombi at the x-ray
- Subcutaneous abscelles at the injection site.
- Palpable enlarged lymph nodes – axillary, cewical or ingwinal
- Froth (occasionally bloodlinged) in the nostrib of mouth
- Cigarette burns of scari on upper chest
- Jaundice
- Evidence of malnutrition.
Internal
- Injection sites: Fresh needle puncture concealed under blood spots of tattoos, with sc. Hemorrhage of needle tracts ( skin increased to explode there features of to see needle puncture in view. Se fibrous and absell: thickening and thrombosis veins previously used for injecting (positions excised for microscopy)
- Generalized finding: Generalized viral cognition, dark red blood, signs of septicemia and systemic neeroto
- Lung enlarged and heavy with intem congention of muccosal ademe. Slight acute emphyema froth in the trachea and brochi aspirated material in the mouth, stomach trachea and man brochi and variegated acute changes in the lungi narcotic contn
- Heast: marked dilatation of RV; bacterial endocarditis commonly from staphylococcus aerens; septic embolism; abscesses of infarction.
- Liver: Congestion: hepatomegaly; acute hepatitis; postneuostic cirrhosis postal fibrous
- Lymphnodes: Enlargement of axillous, hepatic and subpylocical
- Brain; cerebral edema; congestion; softening due to septicemia
- Kidney congestion; softening and smelling are to s
- Spleen enlargement: congestion softening
- Complications: If death not from overdose / hypersensitivity it may occur from one of the following complication septic endocarditic, viral hepatitis, postnecrotic cirrhosis. Titanium (organic sc tumor) military TB, Bronchopneumonia, lung abcess, pulmonary fibrosis, malnutrition.
Microscopy
- Microabsesses : brais, heart, spleen, liver kidneys, LN secondary to septicemia
- Chronic hepatitis: Lympocytic infiltrate of postal and peripostal areas with occasiona neutrophils acute hepatitis with necrosis and acute inflammatory cell infiltration.
- Edema and lymphocytic hypaplacia of LN
- Intestitied pulmonary fibrosis. Pulmonary TB; scattered glannlomar of FB type (polarized light urea and see foreign material talc or starch, x-ray diffraction can be use.
- Foreign body granuloma in skin around blood vessels; thrombus phrobitis; organizing thrombus of view
Speciman to be collected
- Tissue from injection site – skin, sc and muscle
- Blood
- Urine
- Liver.





